Is cord still king?
Tissue management for fixed prosthodontics
by Paul L. Child Jr., DMD, CDT
Making an excellent elastomeric impression of tooth preparations still causes a high level of anxiety in a disproportionate number of clinicians, even with the excellent materials and techniques available today. Although making impressions is a routine procedure, clinicians struggle to find a consistent method to manage the soft tissue while making a highly acceptable impression. In some instances, a perfect impression can be made using a specific technique or combination of materials (and occasionally adding a silent prayer, especially for multiple units). After finding success, a clinician would consider deterring from that method with future impressions “dental blasphemy” (Figs. 1 and 2).
Fig. 1 — Maxillary arch using the two-cord technique with Ultrapak (Ultradent) cord soaked in aluminum chloride, sizes 00 and 0.
Unfortunately, a growing number of clinicians (as reported by dental laboratories worldwide) submit unacceptable impressions (Fig. 3). They know their lab will proceed with the case, primarily due to labs’ fear of losing business if they ask clinicians to remake the impressions. This poor communication and dysfunctional relationship leads to increased remakes and cost, patient and clinician dissatisfaction, and potential decreased longevity of the restoration, if the clinician cements it to the tooth knowing it is inadequate.
Fig. 2 — Corresponding impression with Identium (Kettenbach). Making an impression of multiple preparations is one of the most difficult procedures in all of dentistry, and can be very stressful for the patient and dental team.
Despite the increased number of poor impressions, most clinicians sincerely strive to make better impressions and maintain open relationships with their ceramists, so that the ceramists can let clinicians know if impressions require remakes, and if they should search for improved techniques, materials, and devices.
Fig. 3 — Excellent impression using Aquasil (Dentsply), but poor choice of tray. The lab did ask the clinician to make another impression with a full-arch tray.
The purpose of this review article is to discuss the most common techniques, materials, and devices for excellent tissue management prior to making an impression, and to discuss clinical tips on how to avoid gingival inflammation and recession associated with poor tissue management.
Techniques and materials
Cord has been a mainstay in fixed prosthodontics due to its low cost, ease of use, and predictable results. It comes in many sizes, with or without an impregnated hemostatic agent, can be combined with other medicaments extraorally before use, and can be used for most tooth preparations when it is subgingival (e.g., class V restorations, noncarious cervical lesions, cervical and senile root caries, and more). The most commonly used cord systems are from Ultradent, DUX Dental, Premier, and Roeko.
The most popular technique is the two-cord technique, which leaves one cord in the sulcus during the impression. The one-cord technique is still widely used, but research has demonstrated a higher incidence of unacceptable impressions, especially for subgingival margins when placing the cord only once around the tooth. Therefore, many clinicians combine one cord with another material or technique, such as laser troughing (discussed below), VPS-based material (Magic Foam Cord by Coletene Whaledent), cotton compresses (e.g., Comprecaps by Coltene Whaledent), and paste retraction systems with or without a hemostatic agent (e.g., Expasyl or Hemostasyl by Kerr, Traxodent by Premier). In addition, the one-cord technique is excellent for margins equigingival or supragingival to control sulcular fluid more than retract for margin capture.
Fig. 4 — Excessive tissue removal with laser after cord placement.
The paste systems and VPS-based materials identified above have all proven to be excellent nontraumatic techniques for tissue management associated with impressions. However, limitations include the additional time for use (in patients with healthy, nontraumatized gingiva), increased cost, which can range from $2 to $10 per tooth preparation, and large cannulas that make it hard to place the paste into the gingival sulcus.
Fig. 5 — Note that the tissue is healthy after placement of restorations and healing, but there are areas of permanent loss of tissue.
Lasers for tissue management
Clinicians worldwide have rapidly adopted lasers (primarily diode lasers) due to the decreased cost and the need for digital intraoral imaging. The chairside CAD/CAM community (E4D, CEREC, LAVA C.O.S., etc.) has adopted lasers for more than just the hype and appeal to patients. Proper laser use can result in a very clean and dry field without blood and excess moisture. This is primarily due to the quick hemostatic action of lasers on tissue. When used carefully and at the appropriate setting, lasers can be just as fast if not faster than cord placement. However, improper laser use (primarily by those with inadequate training) can result in tissue height post-healing at a more apical level than desired. It is most likely incorrect to call this condition gingival recession, as the more apically positioned gingival crest is due to blatant misuse or iatrogenic dentistry (Figs. 4 and 5). However, with adequate training, lasers can be an excellent adjunct for tissue management in many dental procedures. Excellent laser options come from Biolase, CAO, Discus/Philips, and Ivoclar.
Diode lasers are rapidly replacing electrosurgery. However, electrosurgery can be an effective method if a very small tip is used and caution is used to avoid removing too much tissue, excessive contact with tooth and/or restorations, and potential damage to the supporting bone. If using an electrosurgery device or laser, the tip should be held almost parallel to the tooth surface to avoid severing the crest of the gingiva and removing too much tissue. Parkell offers a low-cost, effective electrosurgery device.
Clinical tips for tissue management with fixed prosthodontics
Margin placement should be based on restoration type, periodontal health and characterization, and esthetics. Subgingival margins continue to be the most frequent technique for impressions for fixed restorations, although in many cases they can be avoided. Improved ceramics and color matching, in addition to excellent adhesive cements, allow for margin placement that is equigingival and often supragingival. Many veneers can now be prepared and placed with an equigingival or supragingival margin, often using no or only one cord (Fig. 6).
Fig. 6 — Veneer preparations using one cord (two were used for the lateral crown).
Rotary instrument tissue damage should be avoided. The cord should be placed after the tooth preparation is nearly complete with margins temporarily supragingival. Next, the margin should be moved apically to be at the same gingival height after cord placement. This technique will result in a margin that is slightly subgingival (~0.5 mm), and will help avoid tissue damage and subsequent bleeding. This technique is preferred when preparing more than three teeth to achieve highly visible anterior esthetic restorations, and for patients with higher risk of recession. For one to two teeth, the retraction cord can be placed before preparation due to minimal time in the sulcus (15 to 20 minutes).
Fig. 7 — Before making a final impression, make sure that the second cord is visible around the tooth for optimum lateral displacement of gingival tissue.
Chlorhexidine rinses can be used before the preparation and impression appointment, and used again seven to 10 days before restoration delivery. Although some will point out the increased cost of this technique, poor patient compliance, and potential interactions of the rinse on the patient’s health, the benefits far outweigh the risks. I recommend that clinicians dispense the rinse from their offices to increase patient compliance. The use of chlorhexidine combined with a thorough prophylaxis and/or periodontal treatment before the preparation will reduce inflammation of gingival tissues and subsequent bleeding upon cord placement.
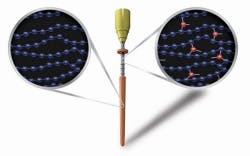
Fig. 8 — One cord combined laser technique. A single cord is placed in the gingival sulcus to expose the inner gingival tissue for laser troughing.
Pack or place? I often observe dentists and their staff members packing cord by inserting it into the sulcus until they feel a high amount of resistance. This technique of packing rather than placing by inserting the instrument parallel to the root surface can result in detachment of epithelium and connective tissue, increased bleeding, and gingival recession. The first cord (if using two cords) should be placed gently into the sulcus with the instrument angled backwards between 45 and 60 degrees (opposite the direction the cord is being placed), so that the cord compresses in on itself and results in both a lateral and apical displacement of the gingival tissue. The second cord should be placed with less force than the first and with the same angulation of the instrument, laterally displacing the gingival tissue so that the entire cord is visible from the coronal view (Fig. 7).
The size of the cord should be as small as possible to adequately displace the tissue for an impression. If using a two-cord technique, I rarely use sizes larger than 00 or 0. For patients with thin, friable gingival tissue, the smallest size should be used to avoid damaging the tissue. For patients with periodontitis and moderate to severe gingival inflammation, it is best to complete initial therapy and reduce the gingival swelling before tooth preparation. However, if necessary, a larger cord may be required to adequately displace the swollen tissue. If combining cord and laser, a size 0 or 1 cord can be placed in the sulcus to expose the inner tooth-facing gingival tissue for subsequent troughing (Fig. 8). Avoid removing excessive gingival tissue from the gingival crest, which can result in further inflammation, patient discomfort during healing and provisionalization, and potential gingival recession. When using this technique, the placed cord may become severed in several places, which warrants caution in removing all pieces.
Fig. 9 — Patient in provisional restorations at three weeks. Notice the blunted papillae, tissue damage, and inflammation caused by aggressive cord packing combined with rough provisionals.
Anterior esthetic and implant restorations require clinicians to understand and characterize each patient’s gingival biotype. Thin biotype as found around some narrow teeth, including many anterior teeth, is predominant in females, and can be more susceptible to gingival recession and future periodontal problems. If using the technique of making an impression of the final abutment intraorally, cord placed gently or careful laser use (mainly in an area with thick gingival biotype) can be acceptable (Fig 9). However, most clinicians prefer to use impression posts (combined with other extraoral techniques such as duplication of the tissue form with composite) to avoid placement of cord and use of laser, which may result in gingival recession. Laser use for gingivectomies and gingival recontouring in the anterior region can be accomplished quickly and predictably. However, I avoid laser use for gingival troughing prior to impressions for anterior esthetic restorations due to increased occurrence of thin gingival biotype, and the potential for subsequent recession and obliteration of too much gingival tissue.
Staff involvement is highly encouraged. Although nondentists cannot use lasers, most areas allow cord placement to be delegated. Teaching assistants to place cord properly can instill a sense of responsibility for excellent tissue management throughout the entire oral cavity, as well as increase efficiency and production for the office. Empowering assistants by teaching them and delegating responsibilities can result in increased staff morale, decreased burnout and job dissatisfaction, and an enhanced team approach to patient care.
Is cord still king?
Cord continues to be a viable and cost-effective method for excellent tissue management associated with tooth preparation and impressions. The cost per tooth preparation of using cord (two-cord technique) and associated hemostatic agents is between 25 cents and 50 cents; thus its continued dominance. However, when used improperly, packing cord can result in gingival recession, unacceptable esthetic results, poor impressions, patient frustration, and increased cost due to lost business and remakes.
Laser use for tissue management is becoming a highly accepted alternative to cord use or in combination with one cord. Improper use of lasers can lead to many of the same negative results as poorly placed cord. Despite the decreased cost of lasers, the cost per tooth preparation can be far higher than cord. To counter this, take courses on laser use to learn the additional procedures lasers can be used for, and this will increase the return on investment. Lasers are quickly becoming an indispensable part of many practices.
Dr. Paul L. Child Jr. is a prosthodontist, certified dental technician, and executive vice president of BISCO Dental Products. He is the former CEO of CR Foundation (formerly CRA) and continues to serve as a board member. Dr. Child lectures nationally and internationally on all areas of dentistry, with an emphasis on new and emerging technologies. He maintains membership in many professional associations and academies, and is on the editorial board of several journals. He can be contacted at [email protected].
Past DE Issues