(CBCT: Does it have a place in general practice?)
By Dr. Bradley Dykstra
For more on this topic, go to www.dentaleconomics.com and search using the following key words: CBCT, general practice, panorex, field of view, Dr. Bradley Dykstra.
When a new technology appears, how do people decide if it is right for them, or when to embrace the advanced technology in their practice? People often erroneously assume that certain technologies (such as panorex in its early years) may be beneficial and practical for specialists or certain types of practices, but not for the average general practitioner. Although CBCT (cone beam computed tomography) is often viewed as one of these conundrums, this is definitely not the case.
It may be easy to visualize the benefits of viewing the three-dimensional images generated by CBCT systems for oral surgeons, TMJ specialists, orthodontists, endodontists, those placing single implants, or those placing multiple implants in edentulous patients. But does CBCT have a place in a general practice that refers out most surgical extractions, endodontic retreatments, and implant body placements?
The answer is an unequivocal yes, especially when we understand and embrace the following reality — even when a patient is referred out for certain procedures, the general practitioner is still the quarterback and should understand the treatment objectives, give guidance to the specialist, and oversee the total treatment process.
CBCT review
As a review for those not familiar with CBCT, it captures volumes or slices of information that are then assembled by software into 3-D views of the scanned area. This allows viewing of the scanned area as a 3-D object as well as viewing from many different angles: frontal, coronal, axial, and transaxial.
This aids in comprehensive diagnostic analysis and presurgical treatment planning. The oral structures dentists work with are three-dimensional, so it is only logical that we be able to view them in the third dimension.
Although cone beam imaging is a relatively new technology for many in dentistry, it has revolutionized the way dentists gather and view information. The result is the ability to diagnose and treatment plan in a manner that we could not even envision a few years ago.
The difference between diagnosing a two-dimensional radiograph to diagnosing from 3-D imaging, which allows for visualization of all structures from any given angle, is truly amazing. The CBCT has forever altered the way many of us practice dentistry. It has not, however, replaced 2-D imaging, but is supplemental to it.
Should a general practitioner embrace and invest in this revolutionary CBCT technology? This was a decision process I had to go through for my practice, especially since I live in Michigan, which has a rigorous certificate of need requirement before acquiring or using any CBCT system.
The CON (certificate of need) program requires the applicant to justify the medical necessity, address the radiation exposure concerns, and provide a cost justification of adding this relatively expensive technology. Going through this process is not without some merit.
After several months of studying the benefits of using CBCT for its increased diagnostic ability and predictability of treatment outcomes, I decided the benefits outweighed the expense of the technology, as well as the cost and numerous hours required to go through the CON process.
In researching the systems, it became clear that the first decision was to choose between the two main options available in CBCT systems — the full field of view or the limited field of view.
One option is considered a large or full field of view, which encompasses most or all of the head. This certainly gives the most information, which is great if it is required, but comes with increased radiation exposure to the patient and with the generally accepted view that the dentist is legally responsible for any pathology present in the scan that may involve the sinuses, brain, spine, or anywhere on the scan. The result is that to be on the legally safe side when using the large field of view, each scan should be read by an oral maxillofacial radiologist, which is an additional cost.
The other option is known as a limited or small field of view system. It encompasses a much smaller area (50 mm x 37 mm for my machine) and is generally confined to the area of interest where the information is required.
The benefits of the limited field of view include a lower cost system, less radiation for the patient, and often no need to have the scan read by a radiologist since it is limited to the dental alveolar areas with which we are familiar. The profession will learn to view and interpret these scans just as it learned to read periapicals and panoramic images. Technologies will soon allow the machines to be adjustable for the specific need — with a small, medium, or full field of view.
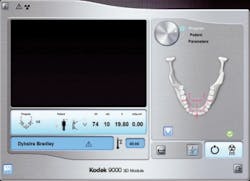
The system I chose was the Kodak 9000 small field of view system. This was the most logical choice for me since I already used the 9000 as my digital panorex machine. By upgrading the machine, I am now able to acquire limited field of view scans that are 50 mm in diameter and 37 mm in height. Image acquisition is as easy as acquiring a panorex, and the software is easy to use. (See Fig. 1)
My experience is that in diagnosing the variety of patient situations that present daily in a practice, this CBCT technology provides much better diagnostic information than I have ever had and has become indispensible.
Following are several cases that demonstrate how this technology has benefited the practice, but more importantly, how it has benefited the patient. I would no longer want to practice without this additional information, which allows me to view each case in the third dimension. The use of CBCT is widely known for implant planning and guided placement, and for extraction of third molars in proximity to the mandibular nerve. However, there are other types of uses that I will present here.
The first case is unusual, but more common than people realize. Part of the practice protocol is taking a digital periapical image of the lower anterior teeth on all adults every one to two years to monitor bone level for early periodontal changes.
At the most recent visit, the lower anterior radiograph revealed significant internal resorption in tooth No. 25. The color of the tooth was normal, as were the pulp vitality tests. A small field of view CBCT image revealed the extent of the lesion and confirmed the resorption had not perforated the tooth exterior. (See Fig. 2) This indicated that appropriate endodontic therapy should be successful. Endodontic treatment was performed uneventfully and the patient was thankful.
Another type of case is often encountered in practice, and that is failed RCTs. It is often unclear why an RCT fails. Small FOV CBCT images of these teeth are very revealing. Periapical lesions previously invisible on 2-D radiographs are easy to see and measure, and cracks or missed canals are also clearly visible. In this case, RCT No. 14 had been performed several years earlier. The patient said it never felt right and was now getting worse. The PA revealed nothing (PA endo). A CBCT was taken of the area and revealed a lesion on the mesiobuccal root. The reason seemed obvious when examining the MB root — there were two visible canals, with inadequate filling in either canal (CBCT endo).
Other very useful finds gained from the CBCT in endodontics included fractured roots, previously invisible periapical pathology, and accessory canals.
At this time, the majority of patients seen in my practice do not require 3-D images for proper diagnosis, treatment planning, or treatment. But for certain cases, two dimensions are not enough and the addition of the third dimension becomes the only predictable way of providing an accurate diagnosis, which enables the correct treatment. This technology is something I would no longer want to practice without.
3-D cone beam imaging, because of the increased amount of information given, is in the process of redefining the standard of care in dentistry. It appears poised to become the standard of care in implant treatment planning. Time will tell where this technology leads in other diagnostic and treatment procedures.
When a general practitioner understands what CBCT is, uses it judiciously, and provides more complete diagnostic information and treatment guidance while involving specialists in the treatment process, everyone wins. The patient receives the most predictable treatment outcome, the specialist has more information than ever before, which improves treatment outcomes, and the general dentist maintains control and orchestrates the complete treatment process.
As health-care professionals, it is important to analyze the use of CBCT scans and all radiography and recognize the radiation exposure for every patient. Guidelines and standards for the appropriate use of CBCT scans are being rapidly developed.
References available upon request.
Dr. Bradley Dykstra is a general dentist in private practice in Hudsonville, Mich. A graduate of the University of Michigan dental school, he earned his MBA from Grand Valley State University. He speaks on integrating technology into dentistry, and consults via his company, Anchor Dental Consulting. Reach him at [email protected] or (616) 669-6600.