Discussing SHORT™ Implants with Dr. Vincent Morgan
For more on this topic, go to www.dentaleconomics.com and search using the following key words: Bicon, SHORT implants, occlusion, Dr. Vincent Morgan.
Editor’s Note: The following is an interview between DE and Dr. Vincent Morgan, president of Bicon.
DE: What is the science behind Bicon’s SHORTImplants?
Dr. Morgan: Wolff’s law of bone modeling and remodeling is the science behind the clinical success of Bicon SHORT Implants with unsplinted restorations. In 1892, Julius Wolff, a German surgeon, published his seminal observation that bone changes its external shape and internal (cancellous) architecture in response to stresses acting on it. Therefore, it is a significant engineering challenge to design a short implant that biocompatibly transfers occlusal forces from its prosthetic restoration to the surrounding bone. It requires the understanding and application of many fundamental biological, mechanical, and metallurgical principles. It is paramount that the entire design of a Bicon SHORT Implant optimizes the effectiveness of each of its features within the implant’s available surface area and length. Clinical success cannot be met by any single implant design feature such as surface area, but rather requires the appropriate integration of all of its features. Bicon’s proven concept for totality of design provides Bicon practitioners with clinical capabilities unmatched by other implant designs.
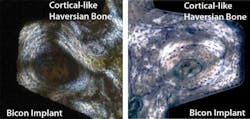
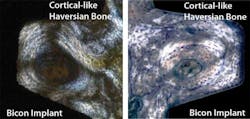
Above left: Histological image of Cortical-like Haversian bone. Above right: Image 6 months after loading, 12 months after implant placement. Courtesy of Paulo Coelho, DDS, PhD, Department of Biomaterials and Biomimetics, New York University. Below: Unsplinted restorations on Bicon SHORT Implants
DE: Why do these implants have clinical capabilities that other implants do not, such as sub-crestal placement and five-to-one crown to implant ratios?
Dr. Morgan: Since an implant’s design dictates its clinical and mechanical capabilities, it is Bicon’s unique design which provides for many of its clinical attributes that are not possible with other implant designs. Bone healing around a Bicon implant is different than the appositional bone (bone that is formed by osteoblasts after cell mediated interfacial remodeling) around threaded implants. An analogy could be made between the mechanical properties of a post in sand and a post in cured cement.
DE: What are the features that distinguish the unique design of these implants?
Dr. Morgan: Since its inception in 1985, Bicon has continuously had three significant design features whoseFirstly, the Bicon implant has a bacterially-sealed 1.5 degree locking taper (galling or cold welding) connection between the abutment and implant, with the ability for 360 degrees of universal abutment positioning. Having a bacterially-sealed connection eliminates the septic bacterial flux associated with clinical odors and tastes, inflammation, and bone loss. As clinicians, we understand the deleterious effects of bacteria on alveolar bone in conventional dentistry. Therefore, is it not logical for clinicians to avoid placing a septic implant connection in healthy bone? Since 1985, Bicon has understood the many benefits of having a connection that is free of bacteria.
The 360 degrees of universal abutment positioning provides for the extraoral cementation of crowns, the use of the cementless and screwless Integrated Abutment Crown™ (IAC), the intraoral bonding of fixed bridges (which eliminates the need for cutting, indexing and soldering of bridge frameworks), multiple and easy removal of abutments over time, and the slight aesthetic rotationaladjustments during and prior to the seating of a restoration.
Secondly, the Bicon implant has a sloping shoulder that facilitates the appropriate transfer of occlusal loads toThirdly, Bicon has had a plateaued, tapered, root-formed implant body since 1985, which provides for 30% more surface area than comparably-sized threaded implants. More importantly, the plateaus provide for an intramembranous-like and faster bone formation (20-50 microns per day) resulting in a unique Haversian bone with different clinical capabilities than the slower forming (1-3 microns per day) appositional bone around threaded implants. Additionally, the plateaus provide for the transfer of compressive forces to the bone throughout the entire implant.
DE: What are the advantages of this innovative design of implants for the dentist and for the patient?
Dr. Morgan: Although the advantages of the simplicity and cost-effectiveness of the Bicon implant are many, I believe the most significant is the greater acceptance of implant treatments on the part of both discerning dentists and patients alike. Because of their short length of 5.0mm and their ability to be used with unsplinted restorations, extensive and expensive treatments involving surgical modalities with morbidities of bone grafting and nerve repositioning as well as complex splinted restorations with custom made attachments and screws can be routinely avoided. Who amongst us would allow a colleague to move our inferior alveolar nerve or take a piece of our hip bone, so that we may have a bicuspid implant? Importantly, when clinicians know that they can easily resolve a metallic-looking gum line with less effort and time than it would take to apologize for its presence, they are more willing to initiate implant treatments. Yes, never again will dentists have to apologize for a metallic-looking implant restoration!
Above left: Image 13 years in function. Above right: Image depicting uniquely different bone. Courtesy of Paulo Coelho, DDS, PhD, Department of Biomaterials and Biomimetics, New York University.
DE: What are the implant lengths that are available and have they been proven by the clinical test of time?
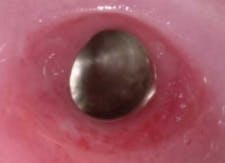
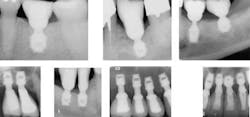
Above: Bicon SHORT Implants avoiding the maxillary sinus. Below: Clinical and radiographic images of a restored Bicon SHORT Implant.
Dr. Morgan: All of Bicon SHORT implants have been proven by the clinical test of time. The 8.0mm SHORT implant has been used continuously, since 1985. The 5.7mm SHORT implant was introduced in 1997. Since 1997, the SHORT implant sizes have been expanded to include 5.0mm and 6.0mm lengths.
DE: This implant has demonstrated bone growth over time. How is this possible?Dr. Morgan: Logically, it has to be because of its design. Bicon does not routinely lose bone; in fact, bone often increases over time around Bicon implants. Rainier Urdaneta, a prosthodontist from Boston, will soon be publishing his clinical research which identifies seven factors associated with bone growth around and over Bicon implants. Interestingly, he notes that shorter implants are more likely to experience bone growth than longer implants. So much for the mantra of "longer is better!" A few of his observed factors are as follows: the implant’s restoration was functionally in occlusion, surface treatment of the implant, and the gingival design of the abutment.
DE: Have you seen increased patient acceptance for implant treatments with the use of these implants?
Above: Prior to (left) and seven years post (right) restoration. Courtesy of Dr. Robert Noone, Camp Verde, Arizona.
Dr. Morgan: Yes, and whenever other dentists can confidently offer a patient a straightforward cost-effective procedure in a timely manner without the inherent risks and expense of surgical bone grafting procedures, they too will experience an increased acceptance of their implant treatments.
DE: How many years have these implants been in use?
Dr. Morgan: Bicon implants have been used continuously since 1985. Any implant or component including the instrumentation that was manufactured in 1985 is compatible with implants, components, and instrumentation being manufactured today.
References available upon request.
Dr. Vincent J. Morgan maintains a private practice in Boston. After placing his first implants in 1970, and years of implant experience with many different systems, he was part of a group that purchased the dental division from Stryker Instruments to form Bicon in 1994. Currently, he serves as president of Bicon, LLC, and is responsible for the development of the Integrated Abutment Crown (IAC). Contact Dr. Morgan at [email protected]
Past DE Issues